by Heather Larson, LSW, CT As a professional caregiver, you may spend more time with the people you care for than your own family. Sometimes the people you care for …
Small communities in a largely rural state, like North Dakota, have an increasing aging population with access to fewer health care resources. Tara Brander, DNP, FNP-C, family nurse practitioner with …
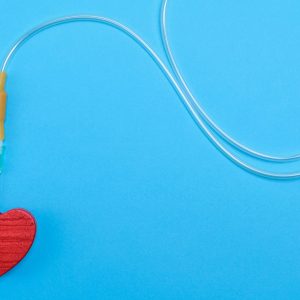
Hospice of the Red River Valley uses a new technology called the Macy Catheter. This specific catheter provides quick symptom management for severe symptoms while avoiding some of the challenges …
For many health care providers working in assisted living facilities, nursing homes and other environments, beginning a conversation about hospice care with a resident, patient or family member can be extremely difficult. Yet, as a trusted source of information, you can play an important role in ensuring patients are informed about—and receive—the most appropriate care available to them.
First, know...